Article
2025 Feb 17
壓力性損傷的最佳實踐與預防方法
壓傷
壓力損傷是由於長期壓力或壓力與剪切力共同作用,對皮膚及下層組織造成的局部損傷。常見於骨性突起處,也可能因醫療設備而產生。
危險因子包括:
- 病患因素:活動能力、感覺知覺、營養狀況、整體健康。
- 外部因素:壓力、剪切力、體溫升高。
- 其他因素:摩擦、濕度、衛生與體位維持時間。
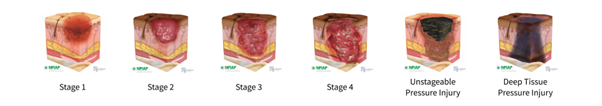
壓力性損傷分級
- 第1級:皮膚完整但呈現不褪色紅斑。
- 第2級:皮膚部分厚度喪失,出現淺層潰瘍或水泡。
- 第3級:全層皮膚喪失,可能見脂肪組織。
- 第4級:全層組織缺損,可見骨骼、肌腱或肌肉。
- 無法分級:因腐肉或焦痂遮蔽,無法判斷深度。
- 疑似深層組織損傷:完整皮膚呈紫色/栗色,伴血泡。
臨床管理與預防建議
重新定位與體位調整
- 檢查所有骨性突起是否獲得壓力釋放,特別是腳跟。
- 建議採用 30° 側臥而非 90°,若無禁忌,可鼓勵 20°–30° 側臥或平躺。
- 重新定位頻率應依患者活動及自主能力調整(每2–4小時皆有效)。
皮膚照護
- 定期評估皮膚壓力點與現有傷口。
- 保持皮膚清潔、乾燥與潤澤,必要時採用隔離產品。
營養補充
對營養不良或風險患者,建議每日攝取:
- 30–35 kcal/kg/天
- 1.25–1.5 g 蛋白質/kg/天
技術輔助方案:減壓床墊 Optima Turn
減壓床墊可作為輔助工具,但不代表唯一選擇。
護理人員角度
- 整合進日常護理工作流程。
- 支援翻身操作,減少約 20% 勞動強度。
- 提供多種氣墊模式(交替氣墊、CLP、轉位模式)。
患者體驗角度
- 兼顧舒適與壓力疏解的治療選擇。
- 穩定翻身速度與角度。
- 氣囊側墊結合床欄,避免滑落與不適。
欲了解更多:Optima Turn 官方頁面
參考資料與進一步閱讀
- Gillespie BM 等 (2020):《體位變換作為壓力性損傷之預防》,Cochrane 系統性回顧。
- 許美玉、林瑞萍、呂基燕 (2019):〈醫療器材相關壓力性損傷預防策略〉,《護理雜誌》66(3): 106–111。
- 馬欣等 (2022):〈末期病人的壓力性損傷與皮膚衰竭〉,《台灣家庭醫學雜誌》32(77‑87)。
- 胡博恩、呂湘婷:〈概論壓力性損傷的預防及治療〉,《家庭醫學與基層醫療》。
- 洪窕淇、劉香蘭 (2019):〈壓力性損傷的營養篩檢與營養介入〉,民生醫院營養期刊。
- 臺大醫院護理部 (2023):《壓力性損傷預防護理指導》。
- 通訊課程團隊:〈壓力性損傷及照護/組合式預防照護實踐〉系列報導(教育訓練與護理實務指引)。